When Life Happens, we’re the Team That Shows Up
Because when you’re in a hospital bed or filling out forms at 2 am, you don’t need a helpline - you need humans who’ll stay till it’s sorted.
Testimonials
Relief, As Our Customers Describe it
We stand by you when it matters most.
swipe
When You Need Us Most, We’re Already There
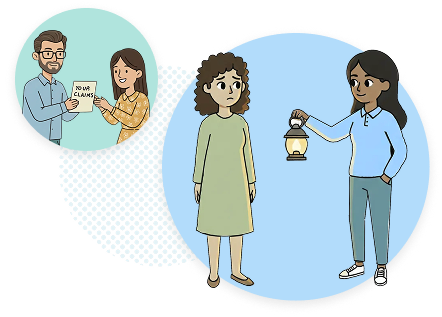
You Tell Us What Happened
We start right away - calmly, clearly, and with no judgment.
We Handle the Messy Bits
Forms, emails, follow-ups, documents, all managed for you.
We Talk to the Insurer
You focus on getting better. We’ll do the back-and-forth.
We Stay Till It’s Done
Every claim ends with closure, not confusion.
The Kind of Care You Need
We translate insurance into human language
We translate insurance into human language
We stick around until AND after the payout - because that’s when support really matters
We stick around until AND after the payout - because that’s when support really matters
We make fairness feel possible - no hidden terms, no silence, no runaround
We make fairness feel possible - no hidden terms, no silence, no runaround
Need to make a claim or understand your cover?
Reach out - you’ll get a real person who listens, explains, and acts fast.